As the new calendar year begins, employers that sponsor group health plans should take steps to stay ahead of key compliance obligations. Several federal reporting and disclosure requirements, mandated under laws such as the Employee Retirement Income Security Act (ERISA), the Affordable Care Act (ACA), and the Health Insurance Portability and Accountability Act (HIPAA), must be addressed early in the year to help avoid potential penalties.
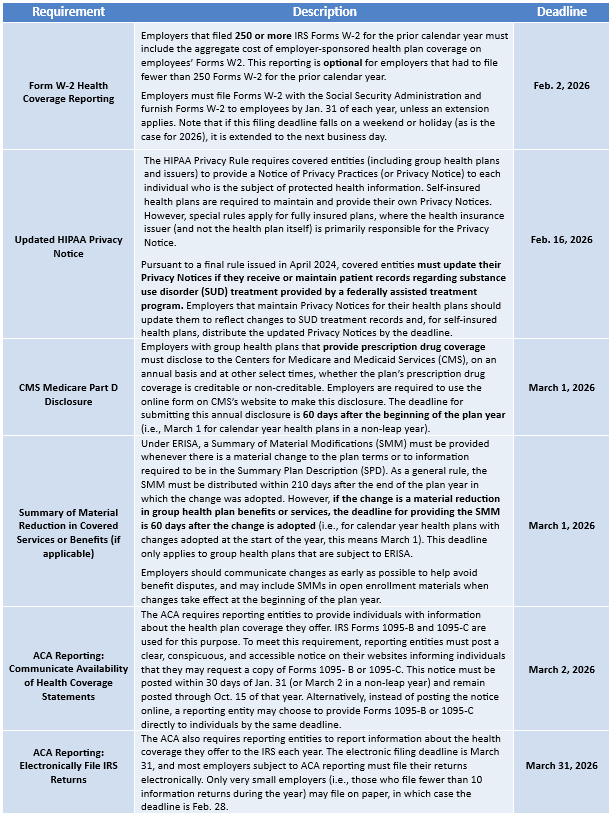
In addition to the deadlines above, the start of the plan year is a good time to confirm that all notices required to be provided at or before open enrollment have been distributed to employees.
Provided to you by Christensen Group Insurance. This Compliance Bulletin is not intended to be exhaustive, nor should any discussion or opinions be construed as legal advice. Readers should contact legal counsel for legal advice. ©2026 Zywave, Inc. All rights reserved.

.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
%20(1).webp)